Gum Recession & Bone Grafting
When there is gum recession, the root of the tooth often shows and is unsightly. Gum grafting is needed to restore health, but root coverage may also be desired to improve appearance. This is generally accomplished with a connective tissue graft, dermis grafts, or the use of tooth development proteins, which help provide new attached gingiva while covering the root surface.
 Recession of canine gum, producing a "fang-like" appearance
Recession of canine gum, producing a "fang-like" appearance Complete root coverage with normal gum contour
Complete root coverage with normal gum contour Front tooth with unsightly root exposed
Front tooth with unsightly root exposed Improved cosmetics after root coverage
Improved cosmetics after root coverage



Root coverage of upper premolars, left and right


Unsightly anterior recession


Recession corrected with root coverage procedure

Bone Grafting
The ideal outcome in the treatment of periodontal disease is to return the tissues to their original state, as they were before the infection started. While we cannot do this in all cases, today more and more pockets can be restored, at least partially, with regenerative surgery. There are three primary types of regenerative surgery:
1. Bone Grafting
The oldest technique used in regeneration surgery calls for placing various materials in the bone defect to stimulate the patient's bone to re-grow. Bone grafting has been used for more than 75 years, but today's materials are much superior in stimulating new bone to form. The implanted material is resorbed by the body, and after 6-12 months has completely disappeared, replaced by new bone. Various materials are available, with the selection made on a case-by-case basis.
 Placing synthetic bone
Placing synthetic bone Synthetic bone placed in defect
Synthetic bone placed in defect Synthetic bone stimulates
Synthetic bone stimulatespatient's natural bone to regenerate
2. Guided Tissue Regeneration
A more recently developed type of regenerative surgery depends on guiding the proper tissue to heal the periodontal lesions. Gum tissue heals very quickly, and after surgery migrates down into the bone pocket quickly. Unfortunately, this does not allow time for the bone to refill the pocket, so the defect persists. With guided tissue regeneration, the gum tissue is excluded from the bone defect with a resorbable membrane, allowing time for the bone to fill back in. This technique has been available for 18 years, and in certain areas is extremely predictable. Click here to see a Clinical Case.
 Defect
Defect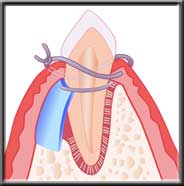 Membrane isolating defect so bone has time to heal
Membrane isolating defect so bone has time to heal New bone forming as membrane dissolves
New bone forming as membrane dissolves Final healing
Final healing3. Cell Stimulation
The most recent development in periodontal regeneration is the use of proteins to induce the formation of tooth supporting structures lost to periodontal disease. Available since 1999, the procedure calls for placing embryonic cells into the defect, which in turn stimulate production of new bone and tissue cells which reform the normal periodontal complex. These cells are porcine (pig), and carry no risk of disease transmission. While long-term studies are not yet available, the research to date warrants use of this approach under certain circumstances.
The periodontist must decide in each case whether the chances of improvement warrant the added expense of bone regeneration. However, restoring bone and the periodontal complex is the gold standard, and periodontal regeneration is being used more and more.